

Innate immunity is the defense system you were born with-and the first to respond to invaders. Senescent cells thus weaken the body and make it harder to fight off infections.īut there’s a lot more going on in an aging body, and many elements of aging likely work together to undermine the immune response, says Eric Verdin, president and chief executive officer of the Buck Institute for Research on Aging, a biomedical research group based in California.Īmong older people, he says, there are two broad abnormalities of the immune system: a hyperactive innate response, and an underactive adaptive response. These cells secrete chemicals that damage neighboring healthy cells and trigger inflammation. But as the body ages, this process becomes less efficient, and it starts to accumulate so-called senescent cells, which are damaged but won’t die. For example, the human body normally clears away cells that have become damaged due to disease, injury, or stress. Scientists who study aging say it likely has to do with some of the hallmarks of getting older. “It’s just one of the great mysteries of the virus,” says Deepta Bhattacharya, an immunologist at the University of Arizona. Aging immune systemsĮxperts say they still don’t have an adequate explanation for why older people were more susceptible to COVID-19 even before vaccines were available.
Here’s what scientists know about the aging immune system-and why breakthrough infections don’t change the fact that COVID-19 vaccines remain remarkably effective for people at any age. ( Why the CDC and FDA only approved booster shots for some Americans.)
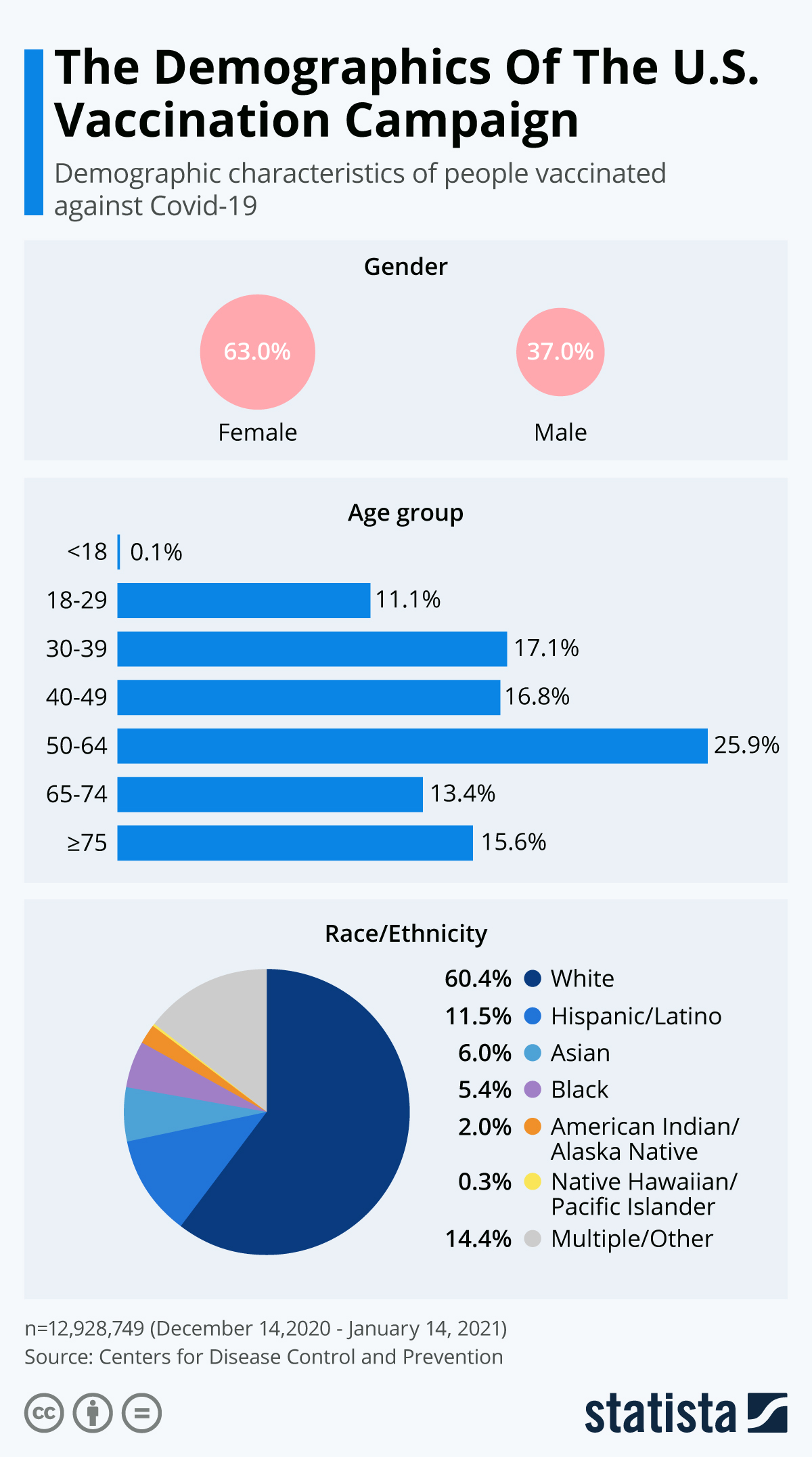
regulators have approved booster doses of the Pfizer vaccine for people over 65-and are poised to do the same for the Moderna and Johnson & Johnson jabs. “If you’re under 45, your chances of dying are almost nonexistent, and then it increases exponentially.”Ĭoncerns over breakthrough infections are also why U.S. prioritized vaccinating older people and those in long-term care facilities when it first rolled out the vaccines, he explains. “The huge risk factor is age,” says William Petri, an immunologist at the University of Virginia.
And recent media reports citing data from Seattle, Washington, and the United Kingdom show that older vaccinated people face similar-and, in some cases, greater-risks of severe disease than unvaccinated children. According to the latest data from the Centers for Disease Control and Prevention, people over 65 account for 67 percent of hospitalizations and 85 percent of deaths from breakthrough cases. People with this form of cancer tend not to respond well to vaccines.īut in addition to the immunocompromised, health officials are seeing worrying evidence that older age groups continue to be at higher risk from the pandemic. Powell was 84, but his cause of death was more complex: The former statesman suffered from multiple myeloma, a cancer of white blood cells. After all, older age brackets have been disproportionately at risk throughout the pandemic, and that continues to be true even once someone is fully vaccinated.Ĭoncerns about breakthrough infections bubbled up again this week when news broke on October 18 that former Secretary of State Colin Powell had died after contracting COVID-19. Mounting data suggest that older people are at higher risk of severe disease from a breakthrough infection of COVID-19-and scientists say that should come as no surprise.


 0 kommentar(er)
0 kommentar(er)
